Be yourself; Everyone else is already taken.
— Oscar Wilde.
This is the first post on my new blog. I’m just getting this new blog going, so stay tuned for more. Subscribe below to get notified when I post new updates.
Be yourself; Everyone else is already taken.
— Oscar Wilde.
This is the first post on my new blog. I’m just getting this new blog going, so stay tuned for more. Subscribe below to get notified when I post new updates.

Rituximab (Rituxan) is a monoclonal antibody used primarily to treat B cell Non-Hodgkin’s Lymphoma. Monoclonal antibodies are laboratory engineered antibodies that are clones of an original parent cell that bind to the same epitope that a normal antibody can. Rituximab is a monoclonal antibody that is used to treat Non-Hodgkins Lymphoma and Chronic Lymphocytic Leukemia. Rituximab, specifically, is able to target B cancer cells by binding to CD20 on the B cells. When Rituximab binds to CD20, it eventually causes the B cell to lyse. The benefit of this is that Rituximab is able to directly kill tumor cells, while also enhancing the acquired immune system’s ability to fight the cancerous cells. To me, Rituximab seems like a promising option for those who have non-Hodgkin’s Lymphoma. For individuals with overreactive and distressed B cells, eliminating unhealthy B cells seems like an effective way of removing tumor cells.
Interestingly, Rituximab works mainly through antibody cellular cytotoxicity. This means that the Rituximab antibodies bind to CD20 on cancerous B cells. By binding, the Fc region of Rituximab is exposed for natural killer cells of the innate immune system to induce antibody cellular cytotoxicity. Rituximab essentially increases the effectiveness of NK cells. Therefore, Rituximab has the benefit of not only enhancing the effectiveness of the innate immune system, but also directly targeting the adaptive immune system via Rixtuximab binding to CD20 of B cells to directly kill cancerous B cells. I find it fascinating to see how monoclonal antibodies like Rituximab are able to integrate the innate and acquired immune system in treating cancer. Rituximab is trying to enhance the actions of the innate immune system, while downregulating the B cells of the acquired immune system. I wonder if there is a way to fine tune Rituximab to increase the expression of CD20 on B cells. I ask this because it seems the downside of this monoclonal antibody would be that if B cells do not express CD20, then there would be no binding site for Rituximab to target.
The main side effects for Rituximab are over stimulation of the immune system due to infusion reactions. This can include hives, fever, swelling, itching, and fatigue. Additionally, Rituxan can cause severe skin or mouth ulcerations. The infusion-related reactions and mouth reactions are most likely to a hypersensitivity reaction, involving IgE antibody. Furthermore, one is not supposed to take Rituximab, while diagnosed with Hepatitis B. Those who take Rituximab, while having Hepatitis B, run the risk of reactivation of the Hepatitis B virus. The reason it makes one more susceptible to Hepatitis B is because the B cells are largely involved in keeping Hepatitis B from being an active infection. Hepatitis B can be a chronic infection, so those who take the drug and lyse B cells are more at risk of having Hepatitis B reactivate. In fact, Rituximab is strongly discouraged from being used in individuals that suffer from any chronic/latent infections. These include Hepatitis C, Herpes Simplex I/II, Varicella Zoster, West Nile Virus, Parvovirus B19, and Cytomegalovirus. Finally, Rituximab is linked to Tumor Lysis Syndrome, which is the abnormally high breakdown of tumor cells. This condition can lead to kidney failure, as well as heart rhythm abnormalities associated with Rituximab. I think the side effects, as well as the certain diseases that Rituximab can make one susceptible to, have to be talked over with a physician. For conditions like non-Hodgkin’s Lymphoma, Rituximab’s benefits may outweigh the side effects. However, again, monitoring of patient’s blood, signs, and symptoms are vitally important in making sure the monoclonal antibody is doing the patient more benefit than harm.

Recent research is starting to shed light on the course of antibody response to Covid-19. According to the research, antibody response to Covid-19 really starts increase exponentially. In fact, on average, by about 9-10 days following onset of signs and symptoms of Covid-19, there was an increase of four fold of IgM and IgG . The typical course of antibodies for Covid is similar to SARs. In patients shortly following signs and symptoms of Covid-19, very low titres exist of either IgM or IgG, but they are mainly IgM. This makes sense, since mainly concentration of IgM would signify that someone has been recently infected with Covid-19. In addition, the data suggests that the median time of class switching of for IgM to IgG is 14 days. Therefore, having higher concentrations of IgM and IgG suggest that someone is further along in the disease progress of Covid-19. I think efficient and rapid testing of IgM and IgG antibodies could play a big role in public health policy in order to identify potential asymptomatic carriers. This would in turn limit the spread of Covid-19 and allow people to social distance when restrictions are ultimately lifted.
In fact, other research looking into a combined IgG and IgM test out of China that identifies a prompt antibody response to Covid-19. In fact, standard testing primarily uses nucleic acid PCR test kits, while this test is an immunoassay that detects IgM and IgG. The primary benefit of this test is that detecting levels of IgG and IgM are able to deduce who is an asymptomatic carrier. Because Covid-19 starts in the lungs, PCR tests can sometimes provide false negatives. However, tracking antibody response through IgG and IgM would be able to identify who is asymptomatic and potentially spreading the virus. I think finding tests that specifically target who is an asymptomatic carrier is vitally important. This is because I think that Covid-19, in particular, is very contagious with a fairly high R naught value. Therefore, early and fast testing is extremely important and will be important to enhance social distancing measures to mitigates the spread of the virus.
Finally, the research that tracked the antibody response of patients infected with Covid-19 provides insight on the importance of identifying people with high concentrations of IgG titres. For example, in this study, following day 20 of infection with Covid-19, IgG titres rose to 1,280 and was the primary antibody present. Individuals with high levels of only IgG antibodies would demonstrate that they have been infected with Covid in the past. This information could be essential in understanding those who may have some immunity to Covid, as well as those who could provide serum antibodies for protection for those who are immunocompromised and need the antibodies. Therefore, I find it quite promising that research into the antibody response to Covid-19 may be the first step in determining effective therapy for the immunocompromised populations. This is certainly relevant because it is this population that we need to protect from Covid-19 as soon as possible. Overall, I think that finding the most efficient, sensitive, and specific will continue to be vital , especially in the short term, to mitigate the incidence of Covid-19 in the future.
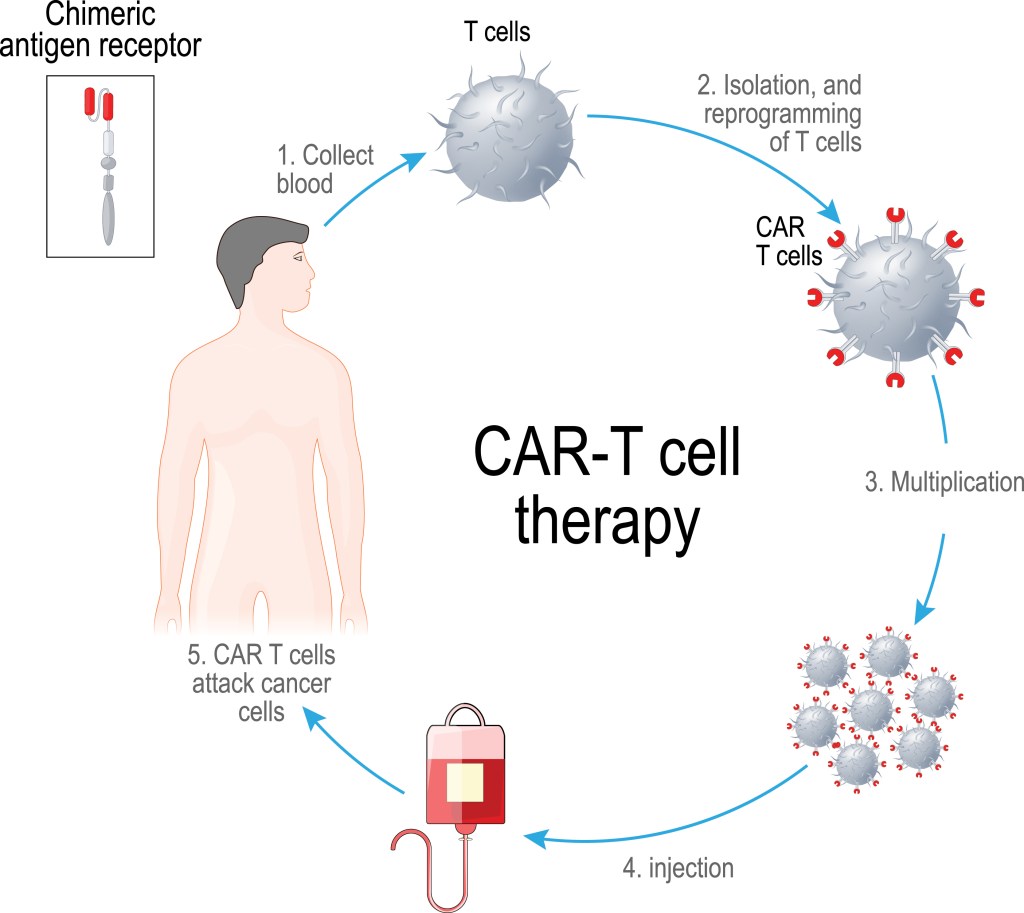
The main topic that I am investigating with this blog is the use of various T cell therapies to tackle cancer treatment. One way that T cell therapy has been adopted to treat is cancer is through T cell receptor therapy. It works because TCR T cells have both alpha and beta domains that activate cytokines. The cytokines then either prevent the expansion of cancer cells or target certain assembly proteins of cancer cells via cancer specific major histocompatibility complex molecules. Another type of T cell therapy that is currently being explored is Chimeric Antigen Receptor T cell therapy, which is generated from a single chain variable fragment of the extracellular domain recognizing tumor associated antigens, as well as an intracellular recombinant motif. When these components are placed into recombinants plasmids in vitro, the plasmids are transduced into the T cells. The major advantage of CAR-T cells then is that they can target tumor cells without MHC.
I think this line of research is appealing and interesting in how we can genetically engineer T cells to target specific antigen on tumor cells. Additionally, by having T cells that are engineered to kill tumor cells without needing the expression of MHC molecules, this has significant benefit for tumor cells that can evade the immune system with decreased expression of MHC molecules. I think this research is particularly pertinent to people who are immunosuppressed. Some research has suggested that CAR T cell therapy is effective in treating viral infections for immunosuppressed patients. This is accomplished by substituting virus-specific T cells with T cells engineered with pathogen-specific CARs. This could be a valuable treatment option for those with underlying conditions.
Some of the disadvantages of CAR T cell therapy and T cell therapy is general are the potential side effects. These side effects include neurotoxicity, cytokine storm release, as well as off-tumor toxicity. In addition, the production of CAR T cell therapy is expensive and requires specialized staff. CAR T cells can unintentionally target normal human tissue cells, which can lead to organ damage. Sometimes, the proliferation of CAR T cells with a massive release of cytokines can induce tachycardia, hypotension, and fever in severe cases. Therefore, while it seems to me the preliminary research on CAR T cell therapy and T cell therapy is promising, it will be important, in my opinion, to monitor the risk/benefit in deciding if it an appropriate treatment measure, depending on the circumstance. That being said, I think CAR T cell therapy could be a new way to tackle cancer treatment and certain viral infections with more efficacy than previous options.

Right now, I am feeling anxious about the coronavirus. Looking at the latest numbers from Johns Hopkins University, we have currently 69,246 cases with 1,049 deaths due to Covid-19. It almost feels like a scene out of “I Am Legend”, where Will Smith plays a US army virologist trying to find the cure for a re-enginnered measles virus that has wiped out 90% of the population and the other 10% turning into cannibalistic Nightseekers. The Nightseekers try to kill the 0.2% of the population that remains immune to the virus. The unaffected immune have to hide in their home and lockdown at night to prevent the Nightseekers from attacking. While the coronavirus is obviously not as severe, it does give me anxiety. I am mainly concerned about my parents, who are older, and the trend of the curve appears grim for the US.
In terms of other aspects of life, the coronavirus has been challenging to deal with. Leaving UNC and saying good bye to some people I will never see again is hard to swallow. The transition to remote learning has not been optimal. Not being able to go to a gym or my favorite coffee shop has taken some of the joy out of my daily routine. There is also uncertainty about how long quarantine from the coronavirus will last. Finally, I feel anxiety about the effects of the coronavirus. This virus will have lasting economic impact on people, as well as the direct effects the virus has on making people sick. I do not think anyone is certain about the exact time frame in which the incidence of coronavirus will decrease. Yet, with all the uncertainty in an unprecedented time, I am keeping optimistic and I keep myself distracted to keep calm.
First, in this uncertain time period, I am making sure I take precautions to ensure that I am doing my part as an individual to slow the spread of potential coronavirus. I am staying in my house as much as possible. I am washing my hands five times a day, at least, for 20 seconds. I am also making sure my mother is not unnecessarily leaving the house to expose herself. In addition, I have been able to get exercise by running in my neighborhood, as well as doing some body-weight exercises for strengthening. Work from remote learning has kept me occupied and I also love to challenge my friends on the Nintendo Switch, when I have time. Also, I have recently gotten into a classic TV series, called Entourage, which came out in 2004. It is about a TV movie star, Vincent Chase, who becomes an A list movie star actor living with his childhood friends from Queens, New York. The group of friends try to make themselves in the Hollywood business out in Los Angeles. These are the simple pleasures that have gotten me through the coronavirus pandemic. Finally, I realize that we will come out of this ordeal stronger. On a positive note, the coronavirus has challenged my perspective on life. It has taught me to realize the many the important things in life, like time with family, time with friends, and the realization that nothing is guaranteed. I will probably never overlook the importance of going to class, or hanging out with friend or family member, after this crisis.
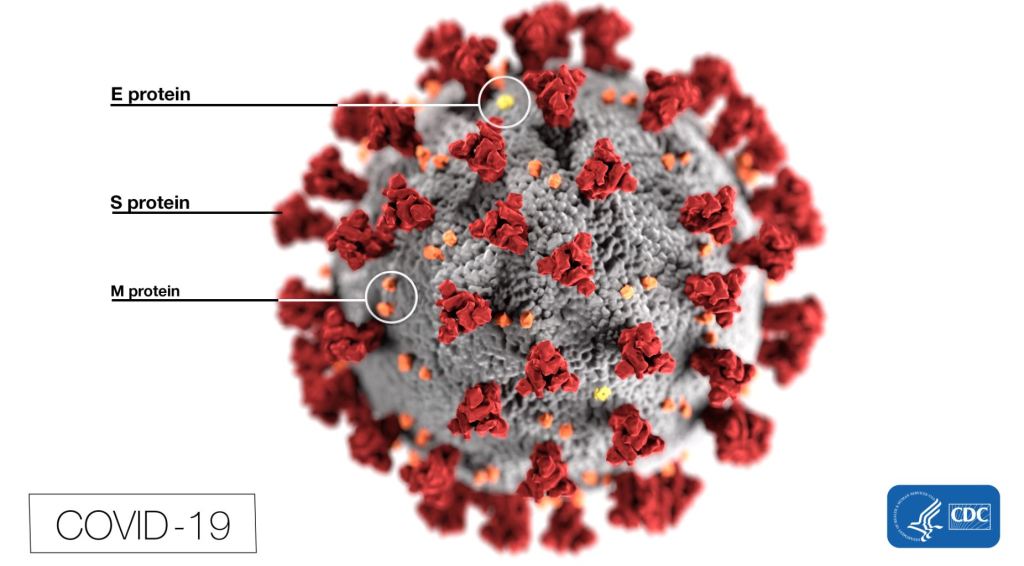
According to Dr. Anthony Fauci, with almost 67,000 cases coming from Hubei province in China, more clarity is beginning to be shed on the novel coronavirus, known as Covid-19. The first 425 cases from Hubei revealed that the median age of infected persons was 59 with a higher fatality and morbidity rate for the elderly and the immunocompromised. The current predicted R0 value of Covid-19 is about 2.2 and the case fatality rate is approximately close to 2%, although predictions believe this number will come closer to less than 1% (Fauci, Lane, & Redfield, 2020). With schools starting to close and travel bans starting to implemented, it will be vastly important to keep social distancing to blunt the growth curve of the virus. It is encouraging to see that policy is starting to really force people to take the coronavirus seriously and keep social isolation to prevent transmission. However, I am concerned with some of the media coverage of the coronavirus. I think simply saying that the youth are not impacted by the virus is misleading because it gives the impression that the youth are more exempt from practicing safe habits. We need to promote social distancing, even in youth populations, to prevent the transmission of the virus to more vulnerable populations. It is just as important for the youth to follow CDC prevention guidelines in slowing the transmission of the virus.
Specifically looking at North Carolina, according to the CDC updates, there are currently 32 cases of Covid-19 cases as of March 15 with 0 deaths. The majority of the cases are coming from Wake county, with 14 cases originating there. According to the most recent CNN news report, the number of coronavirus cases in the US has reached over 3,000 cases with 62 deaths. Recently, Governor Roy Cooper has implemented an executive order banning meetings over 100 people and closing K-12 schools until March 30th. Additionally, we know that Covid-19 can be spread via community and has been declared a pandemic (CDC, 2020). My specific worry with Covid-19 is healthcare facilities and hospitals. Generally speaking, these are locations where a significant population of immunocompromised are held and with known community spread of Covid-19, it is important to keep hospitals as sterile as possible. I think policy restricting visitors at nursing homes and hospitals is forward thinking in promoting the idea of social distancing. Furthermore, because it is known that Covid-19 can be spread via asymptomatic individuals, I am concerned that the number of cases of Covid-19 are higher than reported numbers. As more testing becomes implemented, I expect to see a sharp increase in the number of new cases of people with the coronavirus. I think part of the problem that exists now is that it has been hard to implement tests on a wide scale in such a short time period. How can we speed up tests such that we can gather a more accurate count of those who have the coronavirus? It will require more cooperation between government agencies, healthcare facilities, as well as pharmaceutical companies.
In addition to the situation in North Carolina, the World Health Organization has warned that the lack of personal protective equipment has put healthcare workers in particular danger. The WHO has predicted that 89 million masks, 76 million gloves, and 1.6 million googles are going to be needed each month for the Covid-19 pandemic (WHO, 2020). We need to incentivize the manufacturing industry to increase supply for healthcare workers to be able to tackle the infection. I believe it is much harder to stop the transmission and deal with Covid-19, if healthcare workers do not have the necessary protective equipment to treat the infection. How do we convince the public that panic buying and hoarding actually are contributing to the worldwide shortage of PPE? How do we educate globally that healthcare workers should have priority in being able to obtain personal protective equipment in being able to treat those most affected by Covid-19? Again, national policy in the coming days will be vital in increasing manufacturing of PPE to be able to combat Covid-19.
Interestingly enough, researchers are starting to uncover the antibody response of HSV-2. Specifically, individuals, who demonstrate higher frequency of genital herpes or HSV-2 reoccurrence, were more likely to show higher levels of systemic T cell activation that was HSV-2 specific (Holub et al., 2020). Furthermore, the researchers used interferon gamma assay to indicate that T cell activation was specific to HSV-2. The most interesting component of their results, however, were that the researchers were not able to deduce that the latent infection caused by HSV-2 mounts to higher levels of CD8+ T cells (Holub et al., 2020). To me, this finding is particularly strange given that CD8+ cytotoxic T cells are known to provide immune surveillance, even in latent infections. This could be explained as a result of the localized impact that HSV-2 has on the genitalia region, as opposed to HIV, which mounts more of a response in peripheral immune cells. Overall, this research appeals to me because if we can deduce the molecular mechanism as to what immune response HSV-2 mounts, we may be closer in being able to develop vaccinations and effective antiviral therapy to counteract the sexually transmitted disease. Is it possible to further develop vaccines to target the specific HSV-2 T cells that are naturally higher in recurrent genital herpes reoccurrences? This is one of the questions that I had as a question for further investigation with respect to this specific research.
The other aspect of HSV-2 I wanted to mention in this blog was how HSV-2 makes one more prone to HIV infection. Recent research has illuminated to the fact that HSV-2 actually changes dendritic cells molecularly to allow for productive HIV infection. Intriguingly, HSV-2 works on dendritic cells by activating the cGAS-Sting pathway. The effect of HSV-2 on this pathway ultimately decreases the level expression of signaling proteins, mainly interferon genes like STING and IFI16 (Crisci et al., 2019). Additionally, HSV-2 increases protein breakdown of HIV restriction factors (Crisci et al., 2019). I personally found this research interesting because it shows connection to how HSV-2 makes one more susceptible to HIV. On a molecular level, we see changes to dendritic cells that actually make transmission and infection of HIV more favorable. Therefore, we see how sexually transmitted diseases like HSV-2 can lead an individual to be more susceptible to subsequent infection. This also highlights the fact that immunocompromised populations are especially at risk, once they contract HSV-2, because HSV-2 further works to compromise the immune system.
Furthermore, I think is interesting to see how HSV-2 affects the complement system with PRRs (pathogen recognition receptors). As stated above, the cGAS or cyclic GMP-AMP synthase, upon detecting cytosolic viral DNA, will bind to directly to interferon genes that promote the synthesis of interferon beta (Crisci et al., 2019). This allows for the body to stimulate an effective inflammatory response. I think it is particularly fascinating that somehow HSV-2 interferes with this signaling pathway and prevents the body to mount an effective immune response. In essence, HSV-2 could be a gateway that allows for opportunistic pathogens to take advantage of a compromised immune system to establish a secondary infection. This illustrates to me, at least, the need for more research into finding more effective antiviral therapy for HSV-2 to limit the pathogenesis of the sexually transmitted disease. This blog certainly gave me more insight into the questions of the molecular mechanism in which HSV-2 operates, as well as the certain populations that HSV-2 puts at risk. How can we limit the transmission of HSV-2 and HIV for those who are immunocompromised, asymptomatic, as well as those who are more likely to come into contact with the sexually transmitted diseases?

Particularly in Europe today, the presence of multi drug resistant bacteria is becoming an increasingly concerning problem in health care settings. In fact, superbugs, which antibiotics were normally able to treat, have become resistant to almost all antibiotic options. In one research study, European intensive care physicians have become increasingly concerned with the family of Enterobacteriaceae, especially Klebsiella pneumonia and E. coli. In fact, respondents of the study said that third-generation cephalosporin resistant bacteria, methicillin resistant Staphylococcus aureus, and carbapenem-resistant bacteria were the most prominent emerging superbugs in the intensive care unit. With almost no viable antibiotics to effectively target these drug resistant bacteria, I am concerned whether antibiotic development is staying on pace with the rate at which bacteria are becoming resistant. We need more funding on a national and global scale to initiate research in order to combat the problem of antibiotic resistance. More attention and urgency needs to be placed on our government officials to enact policy and increase spending on newer antibiotic initiatives. Otherwise, populations like infants and the elderly will be at serious risk in the future.
Europe describes the problem of superbugs as a multi-factor problem. One big problem is that patients, who carry multi drug resistant bacteria, have been treated across country borders. As a result, the spread of multi-drug resistant bacteria across borders in Europe is problematic. Additionally, health officials believe that there is more transmission of high-risked bacterial clones in health care settings. Finally, one of the most important issues, according to European physicians, is that antibiotics simply have been misused and overused. Given that most physicians in Europe responded that “they do not have access to last-line antibiotics”, antibiotic resistance and superbugs are incredibly concerning for those who are immunocompromised in health care settings where infections are transmitted easily (Lepape et al., 2020). I think it is important to consider; how do we refine practices such that we are limiting the use of antibiotics in an appropriate manner as health care providers? How can research advance in staying on pace with the rate that bacteria and superbugs gain resistance? How can we refine clinical practices to limit the transmission of future superbugs? These are some of the questions that I am curious about with regards to antibiotic resistance in the future.
The World Health Organization is calling for urgent action to tackle the problem of antibiotic resistance. The World Health Organization echoes concerns that of the 32 priority pathogens, E. coli and Klebsiella pneumoniae are particularly worrisome given that these bacterial infections circulate among immunocompromised people, the elderly, and infants in hospital care settings. Additionally, the World Health Organization is concerned about a highly resistant NDM1 (New Delhi metallo-beta lactamase 1) that many isolates of superbugs now have (World Health Organization, 2020). This specific beta lactamase makes bacteria resistant to a broad spectrum of antibiotics, including carbapenems. Unfortunately, the newer innovative antibiotics against superbugs are either too early in their development stage to be safely tested on patients, or they have shown signs to only be marginally better than current options. The lack of private investing and innovation are critical challenges that the World Health Organization sees to the problem of antibiotic resistance. Therefore, I am curious as to how we can incentivize pharmaceutical companies to continually develop new antibiotics. Are there certain measures to speed up and reduce costs for pharmaceutical companies to develop new antibiotics against multi drug resistant superbugs? This would incentivize pharmaceutical companies, while tackling a problem that could have severe consequences across the world.

Research is being done to see if sequential administration of inactivated polio vaccine (IPV) with oral polio vaccine (OPV) reduces cases of vaccine associated paralytic polio and vaccine-derived polio virus (Ciapponi et al., 2019). The motivation behind the research is to see if there are ways to prevent the severe side effects that can occur with OPV alone. Since OPV is an attenuated virus, it does have the ability to gain virulence after multiple rounds of replication. Therefore, it is interesting to see that the World Health Organization is calling for IPV then OPV administration to see if virulence from the OPV administration alone can be reduced. I personally think this research is vitally important because it solves the problem of finding ways to prevent adverse side effects from OPV, while attempting to empirically validate the World Health Organization’s claims that sequential administration of IPV, followed by OPV, is needed to reduce the number of wild type polio cases. The results of the research, however between OPV/IPV alone verse IPV-OPV sequential administration have been mixed. On the surface, it does appear that IPV-OPV is more beneficial than IPV alone, but the comparison between IPV/OPV verse OPV alone is not as conclusive.
The research suggests that IPV-OPV sequential administration may lower the risk of vaccine associated polio virus, but additionally may also weaken certain mucosal immune responses associated with the P2 antibody (Ciapponi et al., 2019). Additionally, it appears IPV-OPV sequential administration could increase polio virus excretion via the fecal route as well compared to OPV administration alone for certain strains of polio virus. On the contrary, IPV-OPV does appear to heighten immune response and decrease fecal polio virus excretion, compared to IPV alone (Ciapponi et al., 2019). This research to me is significant because it may suggest that more research is needed to study the effects of how IPV and OPV are administered. Why is it that IPV and OPV sequential administration weakens immune response, in comparison to OPV alone? Should we be concerned about this in terms of global health policy? I also wonder if it is possible that the incidence of polio could slightly rise if immune response is weakened via this type of administration. In any regard, I think it is important that we continue to develop research models to ensure that we are vaccinating children with the most effective polio vaccine. Given that children under the age of 5 who are not vaccinated are most at risk, we need to ensure that we are not compromising immunity in our vaccine administration to solely counteract the risk of vaccine-associated paralytic polio.
In terms of the international level, the spread of wild polio virus 1 has been of particular concern. The recently published Geneva statement from the World Health Organization mentions that the number of cases of wild polio virus 1 has increased from 28 in 2018 to 113 cases in 2019 (World Health Organization, 2020). The main reason for the higher incidence of wild polio virus has been due to geopolitical factors. Afghanistan and Pakistan have seen increases in cases mainly due to individuals refusing the vaccine and due to lack of accessibility to vaccine programs, as result of security issues. Additionally, these countries have seen increases in vaccine derived poliovirus. I think it is important to consider how can we can vaccinate individuals, amid political unrest. How can we ensure that border cities in areas where geopolitical factors may play a more significant role can get adequately vaccinated. I believe it will require more international cooperation, as well as enhanced security measures for these areas. Furthermore, it is vital that we invest in funding to educate individuals on a global scale regarding the importance of obtaining the polio vaccine. The more we invest in international global health, the more return I believe we will see in polio virus reduction.

We are starting to learn that the gut microbiome has an important association with neurodegenerative diseases. More evidence is suggesting that the brain and the gut have bidirectional communication in which imbalances can lead to severe consequences. The gut microbiome products affects the neural pathways to the brain, while the central nervous system induces major changes to intestinal motility and immunity. Researchers are starting to link that changes to the microbiome can be indicators for neurodegenerative diseases like Alzheimer’s and Parkinson’s disease. For example, in Alzheimer’s disease, there is evidence linking changes to the gut microbiome and impairment of the Blood Brain Barrier (Zhu et al., 2020). In patients with Alzheimer’s, the loss of the normal microbiota has been linked to increased permeability of the blood brain barrier. In addition, other disease complications like diabetes are often associated with increased amyloid peptide plaque concentration in the hippocampus (Zhu et al., 2020). This line of research to me is exciting because it gives insight that potential biomarkers may exist in identifying those at risk for neurodegenerative diseases. If we are able to hone in on exact macromolecule products produced by changes in the microbiome, we may be able to enhance pharmacogenomic therapy. This can allow us to personalize medicine in a way that optimizes a patient’s treatment plan.
Interestingly, certain bacterial products have been shown to be associated with Alzheimer’s disease. In fact, one of the bacterium we talked about in class has particularly drawn attention: Helicobacter pylori. Chronic H. pylori in the gut can lead to neuroinflammation, amyloid aggregation, and hyperphosphorylation of tau proteins. Additionally, high levels of other bacteria, like E. coli, which make up the microbiome are involved in the progression of Alzheimer’s disease, particularly in amyloid fibril production (Zhu et al., 2020). This type of research is enlightening and points to the idea that disruptions to the human microbiome may be implicated in the neural communication pathways. Furthermore, these findings shed light on the need to develop drug therapy, particularly antibiotics, to eliminate the toxic byproducts the microbiome produces. Finally, these associations may suggest that diet, exercise, and other lifestyle habits are important in preventing deleterious microbiome alterations.
Another disease heavily impacted by the human microbiome is Type II diabetes. Research is starting to suggest that certain bacteria present in the microbiome are heavily associated with Type II diabetes, while other bacterial species are protective against Type II diabetes. For example, Bacteriodes, Bifidiobacterium, Faecalibacterium, Akkermansia, and Roseburia are important bacterial genera in reducing the risk of Type II diabetes. On the contrary, Ruminococcus, Fusobacterium, and Blautia bacterial genera in the human microbiome are associated with Type II diabetes (Gurung et al., 2020). It is believed that these bacteria play direct roles in modulating insulin sensitivity. Again, this line of research supports the idea that diet and extrinsic factors can be important in influencing the microbiome. The research suggests that higher soluble fiber diets, instead of high fat diets, are linked to promoting healthy bacterial species, especially in the gut. These toxic bacterial products can interfere and disrupt important cellular functions, like the permeability of the Blood Brain Barrier and glucose metabolism. I think it will be fascinating to see if microbial genetics research will continue to reveal human microbiome biomarkers that are linked to disease pathology. Additionally, how will this type of research continue to impact dietary guidelines and antibiotic development in the future? How can we be definitive in our conclusions that it is the bacteria causing the disease, as opposed to the disease causing disruptions to the human microbiome?
A lot of attention has been given to the coronavirus and rightfully so, but the influenza virus may be more of an imminent health emergency in the US. In a news article published by CNN about the 2019-2020 flu season, Dr. Fauci, the director of the National Institute of Allergies and Infectious diseases, says that in this flu season, there have already been “2,900 deaths due to the flu” (Cohen & Bonifield, 2020). This is not to mention that the number of hospitalizations and incidences of the flu have continued to increase. Dr. Fauci mentioned that this rise started to occur in October with “6.4 million new cases of the flu and 55,000 hospitalizations since that time” (Cohen & Bonifield, 2020). I think part of the problem we as a society that we need to consider is how do we enforce everyone to get the flu shot. States have enacted laws, like in New York, where one is not allowed to attend public school, until they receive certain immunizations. Maybe it is time to consider widespread national legislation to enforce students, elderly in nursing home or hospital settings, and children in daycares to get the flu shot in the interest of public health. Partial immunity from the flu is better than no immunity.
Dr. Fauci not only points out that this might be the worst flu season in decades, but for one subset of the population in particular: children. According to Fauci, “27 deaths have been reported since December 28th” (Cohen & Bonifield, 2020). The B strain of the flu has affected children significantly, as opposed to adults, since adults have more immunity against the B strain. This is because the B strain is a more stable influenza strain and adults develop more antibodies against this strain over time. Again, this points to my point that all children over the age of 6 months should receive the flu shot. We need to educate the general people better regarding the statistics of not receiving the flu shot versus receiving the flu shot. We have to change the notion that people have, regarding the flu, that getting the shot gives one the flu. In essence, part of the problem that exists with the flu shot is more about educating the general public and demonstrating how one’s decision not to get the flu shot could put another immunocompromised individual at risk.
Unfortunately, to make matters worse, the flu vaccine has been particularly less effective this flu season. According to an article in the New York Times, the initial reports have shown that B strain of the Victoria lineage has not been a great match. Influenza due to B strain has appeared earlier in the flu season, which is not typical. Additionally, in line with what Dr. Fauci said, the B strain particularly hits children the hardest. The A H1N1 pmd09 strain, which usually appears first in the flu season, has also been on the rise. However, it appears that the A H1N1 vaccine strain matches well with the influenza A H1N1 strain that is circulating this year, based on initial reports. The A H3N2 was the dominant strain that caused many cases of influenza in the last flu cycle due to antigenic drift, but it still does appear that the emergence of the B influenza Victoria lineage strain has been the most problematic this year. It could be that the B strain, while typically more stable, is displaying more antigenic drift this year. It will be interesting to see how scientists come up with the next flu shot for the next flu season. I would expect that there will be changes to the vaccine strains for the B strains, given that the number of deaths for children has been historically high. Additionally, given that different strains show different levels of effectiveness year in and year out, I am interested in how scientists will be able to refine their predictive models in producing a more effective flu vaccine overall.